Disclaimer: This article is for informational purposes only and does not replace professional medical advice. Patients experiencing similar symptoms should seek evaluation from a qualified healthcare provider.
Paraneoplastic Skin Rash Linked to Esophageal Cancer: Symptoms, Diagnosis, and Treatment
Skin can often serve as a window into what’s happening inside the body. In some cases, an unusual rash may be the first visible clue that a hidden illness is developing. This is especially true with certain cancers, where the immune system’s reaction to a tumor triggers distinct skin changes. One such case involved a 61-year-old male with a history of tobacco use, who presented with difficulty swallowing (dysphagia) and weight loss — classic signs of an underlying esophageal condition. What followed highlights the importance of recognizing paraneoplastic skin manifestations in cancer care.

Case Overview: From Dysphagia to a Rare Rash
The patient had no significant medical history other than a history of chronic tobacco use. He presented to the emergency department complaining of progressive dysphagia and unintentional weight loss. Vital signs were stable, and his initial physical exam was unremarkable.
Further investigation with esophagogastroduodenoscopy (EGD) revealed esophageal carcinoma. A subsequent CT scan of the abdomen showed metastasis to the pancreas, confirming an advanced stage of disease. Treatment was started with carboplatin and paclitaxel chemotherapy, a common first-line regimen for metastatic esophageal cancer.
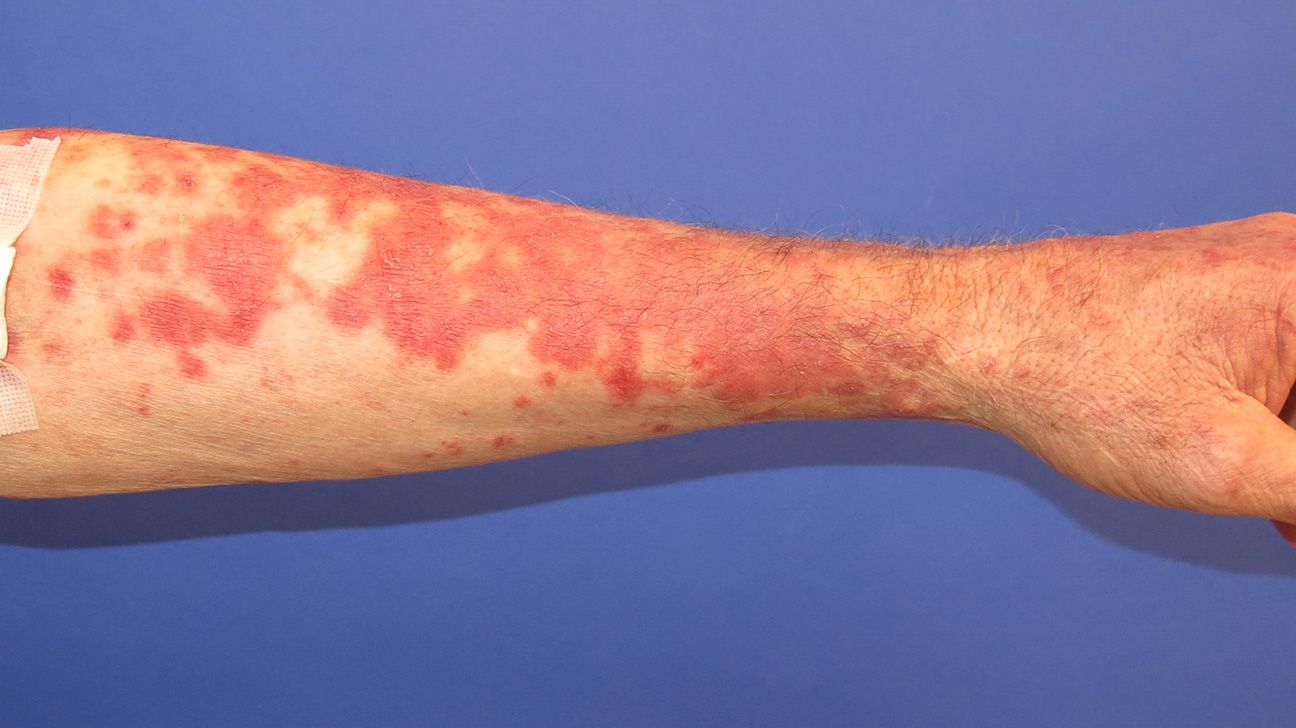
However, about two months into treatment, the patient developed a rapidly progressive pruritic (itchy) rash that started on the left thigh and spread to involve most of the trunk.
Clinical Appearance of the Rash
On examination, doctors noted distinctive serpiginous (wavy) scaling patches with a unique wood-grain appearance. This unusual presentation immediately raised suspicion for a paraneoplastic skin condition.
A skin biopsy was performed. Histopathology revealed:
-
Mild chronic perivascular lymphocytic infiltration
-
Presence of pigmented macrophages
-
Epidermal parakeratosis (retention of nuclei in the stratum corneum)
-
Focal spongiosis (intercellular edema of the epidermis)
These findings were consistent with paraneoplastic figurate erythema — a rare dermatologic manifestation sometimes associated with internal malignancies such as esophageal cancer.

Understanding Paraneoplastic Dermatoses
Paraneoplastic dermatoses are skin disorders that occur as a result of an internal malignancy but are not caused by direct invasion of the cancer into the skin. Instead, they arise due to immune system cross-reactivity, cytokine release, or metabolic effects of the tumor.
The distinctive serpiginous, annular, or wood-grain patterns seen in this patient are considered a cutaneous marker of systemic disease. Recognizing these signs is crucial because they can:
-
Indicate an underlying malignancy that has not yet been diagnosed
-
Serve as a marker of disease progression or recurrence
-
Help guide further investigations and treatment decisions
Risk Factors and Causes
In this case, several contributing factors were noted:
-
Tobacco use is a well-known risk factor for esophageal carcinoma.
-
Advanced malignancy with metastasis can trigger stronger immune responses leading to paraneoplastic symptoms.
-
Chemotherapy may sometimes unmask or exacerbate immune-mediated skin reactions.
Diagnosis
Diagnosis of paraneoplastic dermatoses relies on a combination of:
-
Clinical suspicion – based on the rash’s unique distribution and appearance.
-
Histopathology – confirming inflammatory cell infiltration and characteristic epidermal changes.
-
Correlation with systemic disease – identifying or monitoring an internal malignancy.
In this case, the timing of the rash during chemotherapy also suggested a paraneoplastic or treatment-related immune phenomenon.
Treatment and Management
Management focuses on two aspects:
-
Treating the underlying cancer: Continued chemotherapy is essential to control the primary malignancy.
-
Controlling the skin manifestations:
-
Topical corticosteroids may help reduce inflammation and itching.
-
Systemic corticosteroids or immunosuppressive agents may be used in severe cases.
-
Antihistamines can provide symptomatic relief from pruritus.
-
Close follow-up is crucial, as worsening rash can sometimes signal disease progression.
-
In many cases, improvement in the underlying cancer leads to resolution of the rash.
Prognosis and Clinical Significance
The presence of paraneoplastic skin lesions often correlates with advanced disease and may have prognostic significance. However, early recognition allows clinicians to adjust treatment plans and improve quality of life by controlling symptoms.
Patients should be counseled on skin care, avoiding triggers that worsen irritation, and promptly reporting any new or worsening skin changes during cancer treatment.
Key Takeaways
-
A new, rapidly spreading rash in a cancer patient should always raise suspicion for a paraneoplastic phenomenon.
-
Recognizing the characteristic wood-grain or serpiginous patterns can provide an early clue to systemic disease activity.
-
Treating both the cancer and the skin condition improves patient outcomes and comfort.
-
Interdisciplinary care involving oncologists and dermatologists is recommended for optimal management.
Sources:
-
National Cancer Institute – Paraneoplastic Syndromes
-
American Academy of Dermatology – Cutaneous Paraneoplastic Syndromes
-
PubMed Case Reports: Paraneoplastic figurate erythema in association with esophageal carcinoma